EMERGENCY MEDICAL DISCLAIMER:
This situation could be life-threatening. IMMEDIATELY CALL A DOCTOR or your local EMERGENCY SERVICES number. Do not delay. Your health and safety are the top priority.
what is Infant botulism
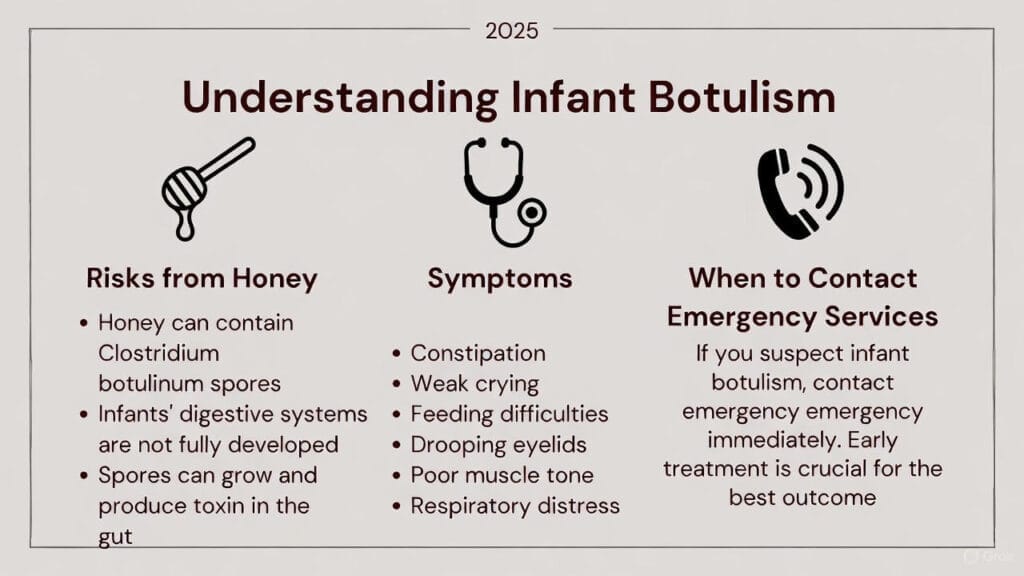
Infant-botulism is a rare but serious illness in babies caused by toxins from the bacterium Clostridium botulinum. Unlike foodborne botulism in adults (where pre-formed toxin in contaminated food causes illness), infant botulism occurs when an infant ingests C. botulinum spores. In the baby’s immature gut, these spores germinate into bacteria that release deadly neurotoxins. In the CDC’s words, “Infant botulism is an intestinal toxemia” caused by swallowed bacterial spores. The toxin blocks nerve function and leads to progressive paralysis. Initial signs are often constipation and poor feeding, but infants can quickly develop lethargy, a weak or altered cry, drooping eyelids (ptosis), and severe muscle weakness (hypotonia). If untreated, the paralysis can descend to the breathing muscles, requiring weeks of hospitalization and possibly mechanical ventilation.
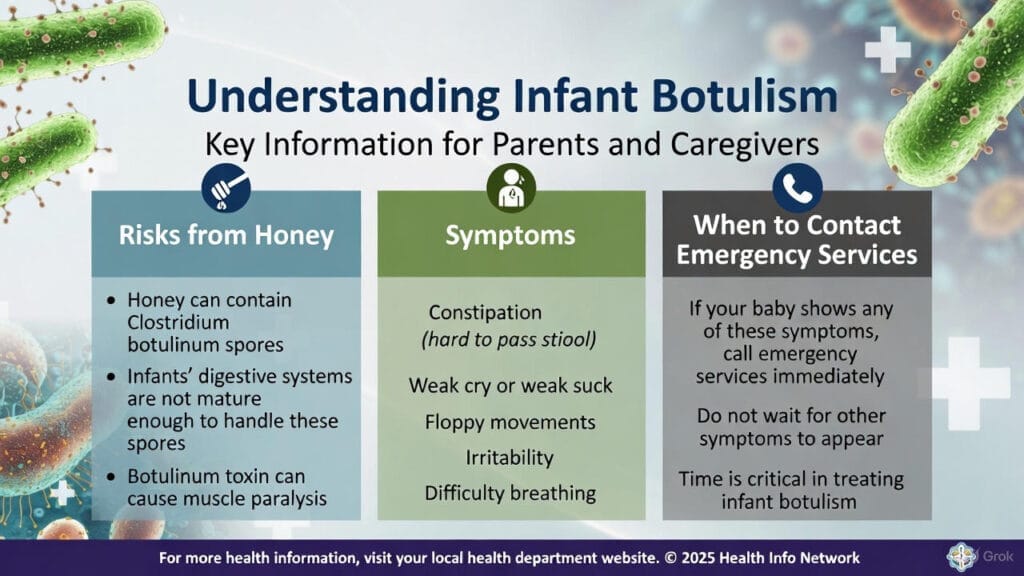
Infant botulism mainly affects babies under about 6–12 months, because older children and adults have gut flora that prevent C. botulinum colonization. The spores are found widely in soil, dust, and some foods. In the past, spore-contaminated honey has been a well-known risk factor – so much so that health authorities warn never to feed honey to a child under 1 year. However, any source of spores in a baby’s environment or diet can trigger illness. Infants may ingest spores from dust, farming environments, or even powdered foods, which can occasionally include formula. In short, infant botulism is a true infection (intestinal toxemia) rather than simply food poisoning by toxin.
“Digital detoxing can have a powerful impact on mental health in just 7 days. By taking a break from screens and social media, you reduce stress, improve focus, and enhance sleep quality. Simple daily steps—like limiting phone use before bed or scheduling tech-free time—can help your mind reset, boost productivity, and improve overall well-being. Learn more about how to get started here: How Digital Detox Can Improve Your Mental Health in 7 Days.”
Causes of Infant Botulism
Infant botulism is caused by Clostridium botulinum spores that an infant swallows and allow to multiply in the gut. The spores germinate into bacteria that produce botulinum neurotoxin in situ. This toxin binds to nerve endings and prevents muscles from contracting.
The classic effects are bulbar palsies and “descending flaccid paralysis,” meaning muscles from the head downward become weak and floppy. The infant’s immature intestinal flora lacks the competition that would normally inhibit these spores, so infection can establish in early life. The CDC notes that infant botulism “occurs when swallowed spores of C. botulinum infect a baby’s large intestine and produce botulinum neurotoxin”for more updates vist GOVT site.
By contrast, foodborne botulism (in older children and adults) comes from eating foods that already contain pre-formed toxin (like improperly canned foods). In foodborne botulism, symptoms usually begin 12–36 hours after ingestion and involve blurred vision, dry mouth, and descending paralysis.
In infant botulism, the toxin is made inside the baby’s gut and symptoms often develop more gradually. Wound botulism is yet another form (from C. botulinum growing in a wound) and is very rare in infants. It is important to recognize that infant botulism is not caused by eating contaminated food toxin, but by an infection in the gut – a key difference noted by WHO and CDC.
Several authoritative sources emphasize that infant botulism is fundamentally an intestinal infection of spores. For example, the CDC explains “Infant botulism happens when swallowed spores from C. botulinum or related species are ingested into a baby’s large intestine and make toxin in it”. Likewise, the WHO points out that unlike foodborne botulism, “infant botulism occurs when infants ingest C. botulinum spores, which germinate into bacteria that colonize in the gut and release toxins”. These definitions underline that preventing infant botulism is about avoiding spore ingestion (e.g. avoiding honey) and maintaining gut health in babies.
Signs and Symptoms
Symptoms of infant botulism typically begin subtly and worsen over days to weeks. Early signs often include constipation (or reduced stooling) and poor feeding, as the baby’s gag and suck reflexes weaken. The baby may seem lethargic or floppy. Other hallmark symptoms are drooping eyelids (ptosis), weak or altered cry, facial expression changes, and loss of head control. The CDC lists common symptoms as “constipation, poor feeding, ptosis (drooping eyelid), sluggish pupils, flattened facial expression, diminished suck and gag reflexes, weak/altered cry, and respiratory difficulty”. Medical sources concur: infants often show weak muscle tone and a “striking loss of head control”, with an altered cry and lethargy. Importantly, these symptoms can initially be mistaken for other conditions, so careful attention is needed.
As botulism progresses, the baby’s muscle weakness spreads. Floppiness may become generalized, and feeding or breathing can become dangerously impaired. Infants may have difficulty swallowing or taking a bottle, and breathing muscles can be affected last, potentially requiring intubation. CDC guidance notes that infant botulism “often starts with constipation but is usually first noticed as difficulty feeding (sucking and swallowing), a weak and altered cry, and loss of muscle tone.”. In short, if a baby under one year old suddenly becomes very weak or has trouble feeding and breathing, infant botulism must be considered.
Key symptoms to watch for include:
- Constipation or decreased stooling – often the first clue.
- Poor feeding or weak suck – baby is too floppy to feed well.
- Lethargy and floppiness – “frog-like” posture, loss of head control.
- Ptosis (drooping eyelids) and decreased facial expression – face may look flat or expressionless.
- Weak or abnormal cry – sounds weak, breathy or strained.
- Difficulty swallowing – may drool or choke on milk.
- Respiratory difficulty – slower breathing or pauses as paralysis worsens.
Any infant with these signs – especially if they have eaten something that could be contaminated – should be assessed by a healthcare provider immediately. Remember, symptoms can develop gradually over several days or weeks, so parents should stay alert if even mild signs appear. As one news advisory warned, “Symptoms can take as long as several weeks to develop, so parents should remain vigilant”.
Diagnosis and Treatment
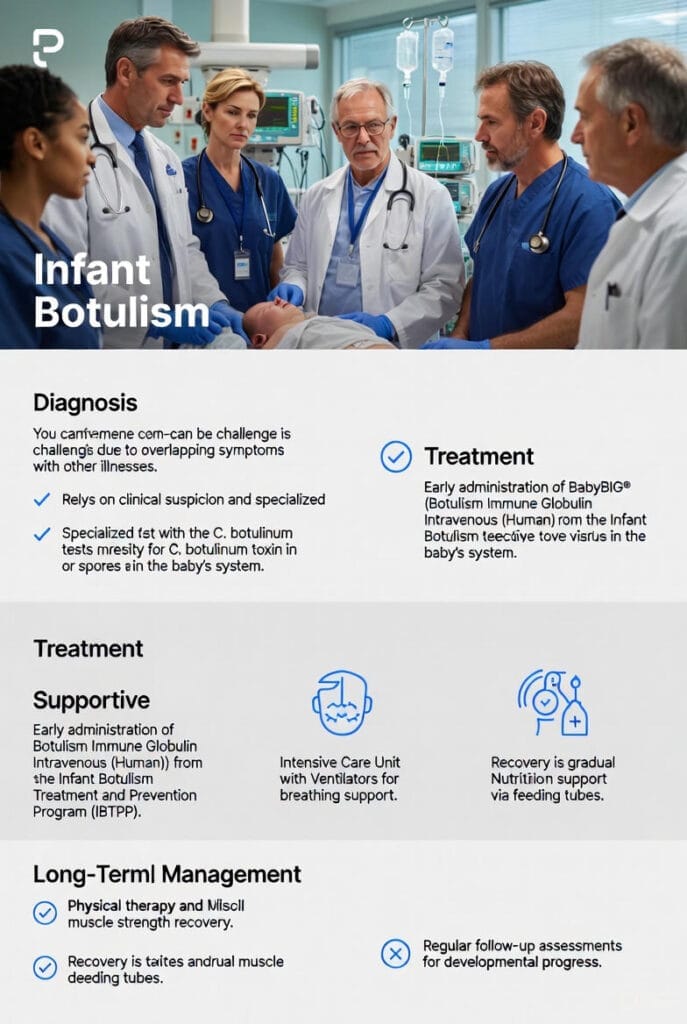
Diagnosing infant botulism is challenging because early symptoms overlap with other conditions. Diagnosis usually relies on a high index of suspicion by clinicians. The CDC emphasizes that “initial diagnosis of infant botulism is based on clinical symptoms”, not waiting for lab results. There are tests (stool or enema specimens sent to public health labs) that can confirm C. botulinum toxin or spores, but these take time. In practice, doctors often start treatment empirically if infant botulism seems likely, rather than waiting for confirmation.
The cornerstone of treatment for infant botulism is BabyBIG® (Botulism Immune Globulin, Intravenous), a human-derived antitoxin available through the California Infant Botulism Treatment and Prevention Program (IBTPP). When consulted, IBTPP provides BabyBIG to neutralize circulating toxin. The CDC advises clinicians: “If clinical consultation supports infant botulism, begin treatment with BabyBIG as soon as it is available. Do not wait for laboratory confirmation to begin treatment.”. Supportive care in an intensive care unit is also critical, as infants often need respiratory support (ventilators) until the toxin’s effects wear off. With prompt BabyBIG treatment, most infants recover over weeks, although full recovery can take a long time. Death is rare when treated, but can occur if treatment is delayed.
Aside from antitoxin, care focuses on nutrition and breathing. While hospitalized, babies are usually fed through tubes and monitored for respiratory failure. Recovery is typically slow; the average hospital stay can be several weeks. Physical therapy may be needed for muscle strength, and long-term follow-up ensures development remains on track. Fortunately, the IBTPP reports that most treated infants eventually regain muscle function, although some may have minor residual issues.
Infant Botulism vs. Other Botulism Forms
It is important to contrast infant botulism with other types. Foodborne botulism (often due to home-canned foods) is usually a sudden illness in older children or adults from eating pre-formed toxin. In foodborne cases, symptoms start within hours to a day of eating bad food. By contrast, infant botulism involves ingestion of spores (not toxin) and the onset can be insidious. Wound botulism (from infected wounds) is very rare in infants and occurs when C. botulinum infects a wound and releases toxin. Also extremely rare is adult intestinal toxemia, which is physiologically similar to infant botulism but occurs in older people with altered gut flora. None of these should be confused with infant botulism, which specifically affects babies.
As WHO explains, “Infant botulism occurs mostly in infants under 6 months of age” and “different from foodborne botulism caused by ingestion of pre-formed toxins in food, it occurs when infants ingest C. botulinum spores”. Adults have defenses in their intestines that infants lack; in healthy adults, swallowed spores usually pass harmlessly. The only proven prevention for infant botulism is to avoid feeding honey to infants under 1 year old. In terms of treatment and recovery, all types of botulism share the need for antitoxin and respiratory support, but infant botulism is unique in requiring the specialized BabyBIG product and public health reporting due to its rarity in babies.
Infant Formula and Botulism Risk
Recent events have drawn attention to the possible link between powdered infant formula and infant botulism. Powdered formula is not sterile and can (rarely) carry bacteria or spores. The CDC cautions that powdered formula “does not need to be warmed before feeding” and notes elsewhere that “powdered infant formula is not sterile and can sometimes have germs (such as Cronobacter)”cdc.gov. Likewise, New York health authorities observed that “Powdered infant formula, while generally safe, can occasionally contain C. botulinum spores.”cbs6albany.com. In other words, formula can very infrequently carry C. botulinum from the environment or ingredients.
In November 2025, epidemiologic evidence pointed to a Clostridium botulinum contamination in a baby formula product. U.S. health officials reported 13 cases of infant botulism across 10 states, and all affected infants had consumed the same brand and lots of powdered formulacdc.govapnews.com. The formula in question was ByHeart Whole Nutrition Infant Formula. On November 8, 2025, ByHeart voluntarily recalled two specific lots (codes 206VABP/251261P2 and 206VABP/251131P2, both “use by 01 Dec 2026”) after the CDC and FDA found a strong link to the outbreakapnews.comcdc.gov. The CDC stated that “epidemiologic data show that ByHeart Whole Nutrition infant formula might be contaminated with Clostridium botulinum and has made infants sick.”cdc.gov. Although investigations (lab testing of leftover formula) are still ongoing, this is the first known instance of a powdered infant formula being directly tied to infant botulism cases in the U.S.
Aside from this incident, infant formula has not historically been a source of botulism. The FDA and companies stress that “there is no historical precedent of infant formula causing infant botulism”fda.gov, and note that “botulism is extremely uncommon in dairy products or infant formula”fda.gov. Indeed, in most formula-related recalls (such as recent Cronobacter/Salmonella recalls), botulism was not found. For example, a February 2022 recall of certain Lyons Magnus (Kate Farms, PediaSure) formulas mentioned a theoretical risk of C. botulinum, but testing found no botulism contaminationchop.edu. Similarly, Abbott’s Similac recall (Cronobacter/Salmonella) had nothing to do with botulism. In summary, formula contamination with botulinum spores is rare – but the 2025 ByHeart outbreak shows it can happen, so vigilance is warranted.
There are other documented cases internationally. In 2015, Hong Kong authorities recalled certain milk formulas (Cow & Gate Happy Kid formula) after detecting C. botulinum in a whey protein ingredient from New Zealandcfs.gov.hk. This incident involved a growing-up formula (for toddlers) and a specific contaminated ingredient, but it underscored that Clostridium botulinum spores can enter the formula supply chain. It also highlights that global supply chains (e.g. imported ingredients) are an area to watch. While U.S. recalls in recent years have focused on other bacteria, parents should know that any formula could theoretically carry spores if contamination occurs.
Major recent recalls linked to infant formula include the ByHeart recall in November 2025apnews.comcdc.gov. In all other recent U.S. formula recalls (like Enfamil/Nutramigen in 2023 and Abbott’s Similac in 2022), the concerns were Cronobacter or Salmonellachop.educhop.edu, not C. botulinum. One FDA notice from 2022 even stated that some formulas “might have a risk of having Clostridium botulinum, but this has not been found so far.”chop.edu. No FDA or CDC recalls have been issued solely for botulism risk before 2025. Thus, the ByHeart event is unique, but it serves as an important reminder that all powdered formulas should be prepared and handled with care.
Steps for Parents: Recognizing and Responding
Parents should be especially aware of the signs of infant botulism and what to do if they occur. If your baby has the symptoms listed above (e.g. severe constipation, very poor feeding, drooping eyelids, weakness, difficulty swallowing), seek medical attention immediately. Tell your pediatrician or emergency department that you are concerned about botulism, especially if any baby has consumed recalled formula or honeycdc.govapnews.com. In the recent outbreak, health agencies advised: “If an infant has consumed recalled formula and then had poor feeding, loss of head control, difficulty swallowing or decreased facial expression… seek medical care right away.”apnews.com. Do not wait for symptoms to escalate. Early recognition and treatment with BabyBIG greatly improve outcomes.
If a specific lot of formula is recalled, stop using it at once. Note the lot number and brand in case medical staff need the informationapnews.comfda.gov. Throw out the product or return it as instructed by the recall notice. Clean any feeding bottles, nipples, and surfaces that touched the formula thoroughly with hot soapy water or in a dishwasherapnews.comcdc.gov. The CDC advises washing and sanitizing because even tiny residues or dust from the formula could theoretically carry spores. Although there is no guarantee that home cleaning removes all risk, these steps reduce exposure to any contaminants.
Finally, report suspected cases. Infant botulism is a notifiable disease; healthcare providers should inform local health departments if they diagnose it. If your baby is diagnosed, you or your doctor can also notify the CDC’s Infant Botulism Treatment and Prevention Program (IBTPP). Parents can contact IBTPP directly 24/7 at (510) 231-7600 for consultationcdc.govfda.gov. This ensures swift access to BabyBIG if needed. Reporting also helps public health officials trace the source and prevent further cases.
Safe Feeding and Hygiene Practices
While infant botulism cannot be entirely prevented (since spores are ubiquitous), certain feeding hygiene practices can greatly reduce risk and improve overall infant health:
- Do not give honey to babies under 1 year. Honey is a known source of C. botulinum spores. The CDC is clear: “Honey can contain the bacteria that cause botulism. Do not feed honey to a child who is younger than 1 year old.”cdc.gov. This includes honey in pacifiers or foods. Many infant botulism cases in the U.S. have been linked to honey, so this rule is a top preventive measure.
- Clean and sanitize feeding equipment. Wash hands well before preparing formula. Sterilize bottles, nipples, and feeding tools with boiling water or in a dishwasher if possiblecdc.gov. Clean preparation surfaces thoroughly. Any container, scoop, or utensil that contacts formula should be sanitized, as spores can survive on surfaces. After feeding, wash bottles and pump parts immediately. Some guidelines recommend using a bleach or steam sterilizer for extra safety, especially if a baby is immunocompromised.
- Use safe water and follow prep instructions. If your baby is healthy and over 2 months old, you can generally mix powdered formula with safe tap water at room temperature. However, for newborns, preemies, or during a known outbreak, CDC recommends using very hot water to mix formula to kill germs. In high-risk situations, boil water and let it cool no more than 5 minutes before mixing (around 158°F/70°C)cdc.gov. This step is standard for preventing Cronobacter infections, and it would also help kill some vegetative bacteria (though C. botulinum spores require higher heat to inactivate). Whether you boil water or not, always follow the formula label’s directions exactly: measure water first, then add powdercdc.gov. Never dilute formula beyond instructions, and use clean measuring tools.
- Store formula properly. Unopened formula should be kept in a cool, dry place (pantry or cupboard), not in a car or humid areacdc.gov. Once you open a container, tightly close it and write the date opened on the lid. Most powder should be used within 1 month of opening, as per label instructionscdc.gov. Prepared formula should not sit at room temperature for more than 2 hours – use it or refrigerate it within that timecdc.gov. Discard any leftover formula after feeding; saliva can introduce bacteria into stored formula.
- Be cautious during recalls or outbreaks. Keep informed about any FDA or CDC alerts. If a formula recall is issued, follow the recall instructions exactly. Sign up for FDA or CDC email alerts (like CDC’s Botulism email updatescdc.gov) to stay current. In the November 2025 case, New York’s health department advised parents to “immediately stop using any recalled formula and follow the FDA’s instructions for safe disposal or replacement”cbs6albany.com. Likewise, thoroughly clean any areas or utensils that may have contacted the affected formulaapnews.com.
- General feeding hygiene: Always wash your hands before feeding your baby or handling formula. Clean surfaces, highchairs, and toys regularly to reduce exposure to dust. Remember that C. botulinum spores can be found in household dust and soilcdc.gov. While you can’t sterilize the entire home, keeping floors and carpets vacuumed or swept helps reduce environmental contamination. If your baby crawls or mouths objects, be aware of where they play.
- Consider alternatives in high-risk cases: If your baby is at especially high risk (e.g. under 2 months, preemie, immunocompromised) and there is concern about powdered formula, discuss alternatives with your pediatrician. Ready-to-feed liquid formula is sterile and avoids the powder-processing issue, though it is more expensive. Of course, breast milk (donor or expressed) is sterile at point-of-consumption and contains maternal antibodies; exclusively breastfeeding until 6 months is recommended when possible, both for nutrition and lower infection risk. However, if formula must be used, strict hygiene is vital.
Following these guidelines not only helps prevent botulism but also reduces other infections (like Cronobacter and Salmonella). As the CDC emphasizes for powdered formula: “Powdered infant formula is not sterile” and precautions can protect your babycdc.gov. In the unusual event of a botulism-linked recall, having good habits in place means you can act quickly to remove any risk.
Prevention Tips and Updated Guidance
- Check Official Sources: Regularly check FDA’s Infant Formula Recall webpage and CDC’s botulism updates for current informationcbs6albany.comcdc.gov. FDA and CDC information will list specific products and lot numbers if needed. For example, the November 2025 FDA advisory clearly listed the affected ByHeart lot codesfda.gov and gave instructions on what to do.
- Talk to Your Doctor: If you have concerns—such as unusual lethargy in your baby, persistent constipation, or any feeding problems—call your pediatrician.
- Mention any potential exposures: (like formula brands, baby’s food history, or honey ingestion). Doctors can then decide whether to consult CDC’s IBTPP or order diagnostic tests.
- Stay Calm and Informed: It’s natural to worry about headlines of botulism cases. Remember that infant botulism is still very rare. In most years the U.S. sees only ~100 cases nationwide. While recent outbreaks raise awareness, thousands of babies safely drink formula without issues every day. Follow safety steps and keep your baby’s routine as normal as possible. Breastfeeding mothers, or those mixing formula, should continue good hygiene but need not panic.
- Symptom Monitoring: Even after stopping any suspect formula, continue to watch your baby. In the recent outbreak, CDC warned that symptoms “can take as long as several weeks to develop” after ingestioncdc.gov. So if your child consumed a recalled formula, be extra vigilant for several weeks. If symptoms occur at any time, seek care immediately.
- Education and Advocacy: Share accurate information with other caregivers (grandparents, babysitters, daycare providers). Make sure everyone knows not to feed honey, to prepare bottles safely, and to wash hands before feeding. Preparedness can prevent many issues. In case of a recall, help coordinate returns of affected formula and spread the word to your community.
Conclusion
Infant botulism is a life-threatening condition, but it is preventable in many cases with proper precautions and early action. Parents and caregivers should understand its causes and symptoms, and be especially mindful of recent outbreaks linked to powdered formula. By learning the signs—such as poor feeding, constipation, floppy muscles, and weak cry—families can seek help without delay. Following recommended infant feeding practices (proper hygiene, no honey, safe formula prep) will greatly reduce the risk of toxin-producing bacteria.
The recent recall of ByHeart Whole Nutrition formula emphasizes the importance of vigilance. CDC and FDA continue to investigate these cases; the companies involved and public health agencies are working to ensure no more contaminated product reaches infantscdc.govfda.gov. Health authorities stress that all parents of infants should “remain vigilant if they used the recalled lots” and should follow up with medical care if any symptoms appearcdc.govapnews.com.“Research-backed. Fact-checked. Trusted by readers.”
Finally, always keep lines of communication open with your baby’s doctor and local health officials. If anything feels wrong with your baby’s health or feeding, do not hesitate to contact medical help. In the case of any suspected infant botulism, the CDC recommends immediate consultation with the Infant Botulism Treatment and Prevention Program. With prompt recognition and treatment, infant botulism can be managed effectively. By staying informed and practicing safe feeding, families can keep their infants healthy and prevent this rare but serious illness.
Lumechronos: Our Commitment to Accuracy and Your Safety
At Lumechronos, our content is the product of meticulous, independent research and is rigorously fact-checked against leading global health authorities like the CDC, WHO, and FDA. We are dedicated to a continuous review process to ensure the information we provide is both current and transparent.
A Vital Note for Our Readers:
The articles on this blog are intended for informational and educational purposes only. They are developed through research and synthesis of publicly available data and should not be considered a substitute for professional medical advice, diagnosis, or treatment.
In a Medical Emergency:
If you or someone else is experiencing a health crisis, immediately disconnect and contact your local emergency services or go to the nearest hospital. Do not rely on online information in such situations.
For General Inquiries:
For non-urgent questions or further support, our team remains available 24/7 via WhatsApp and email. We are here to assist with your informational needs.
This article was developed by Abdul Ahad and the Lumechronos research team through a comprehensive analysis of current public health guidelines from trusted institutions. Our mission is to provide well-sourced, easy-to-understand information.
Important Note: The author is a health content researcher, not a doctor. For medical advice, please consult a healthcare professional.